8
INTRODUCTION
While the diversity of the American population is one of the Nation’s greatest assets, one of
its greatest challenges is reducing the profound disparity in health status of America’s racial
and ethnic minorities and other health-disparity populations compared to the population as
a whole. Among the noteworthy findings in their 2002 report entitled
Unequal Treatment:
Confronting Racial and Ethnic Disparities in Health Care
, the Institute of Medicine concluded
that, even when disease severity, socioeconomic status, education, and access are controlled
for, racial and ethnic minorities receive lower quality health care, including routine services,
compared to Whites, and these differences are associated with worse clinical outcomes.
1
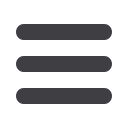
Musculoskeletal disparities threaten
the health of the nation. One in
five Americans suffer from doctor-
diagnosed osteoarthritis, but among
three segments of the population,
the impact is worse. Women, African
Americans, and Hispanics/Latinos
have more severe arthritis and
functional limitations. (Note: Unless a
study specifies a particular population
such as Mexican American, this document defines Hispanics/Latinos per the U.S. Department of
Health and Human Services Office of Minority Health as follows: “This ethnic group includes any
person of Cuban, Mexican, Puerto Rican, South or Central American, or other Spanish culture
or origin, regardless of race.”)
2
These same individuals are more likely to be obese, diabetic, and
have a higher incidence of heart disease - medical conditions that can be improved with physical
activity. Instead of moving, however, these groups have an inactivity rate of 40–50 percent
and this rate is going up!
3
According to a 2010 report from the Centers for Disease Control
and Prevention (CDC), 22.2% of adults aged ≥18 years had self-reported doctor-diagnosed
arthritis, and 42.4% of those with arthritis
had arthritis-attributable activity limitation
(AAAL). Among persons who are obese, an
age-adjusted 33.8% of women and 25.2%
of men reported doctor-diagnosed arthritis.
The CDC notes that while arthritis and AAAL
represent a major public health problem in
the United States, it can be addressed, at
least in part, by implementing proven obesity
prevention strategies and increasing the
availability of effective physical activity programs and self-management education courses in
local communities.
4
The role of the nurse in managing a patient’s risk and progression of osteoarthritis (OA) has been
evolving and can include evaluation, education of the patient, risk management for medications
and other management activities, care coordination among the patient and healthcare
professionals, and compliance strategies including proper medication use, weight reduction,
W
omen in the Framingham
OA study who lost 11 lbs.
reduced their risk of symptomatic
knee OA by half.

















